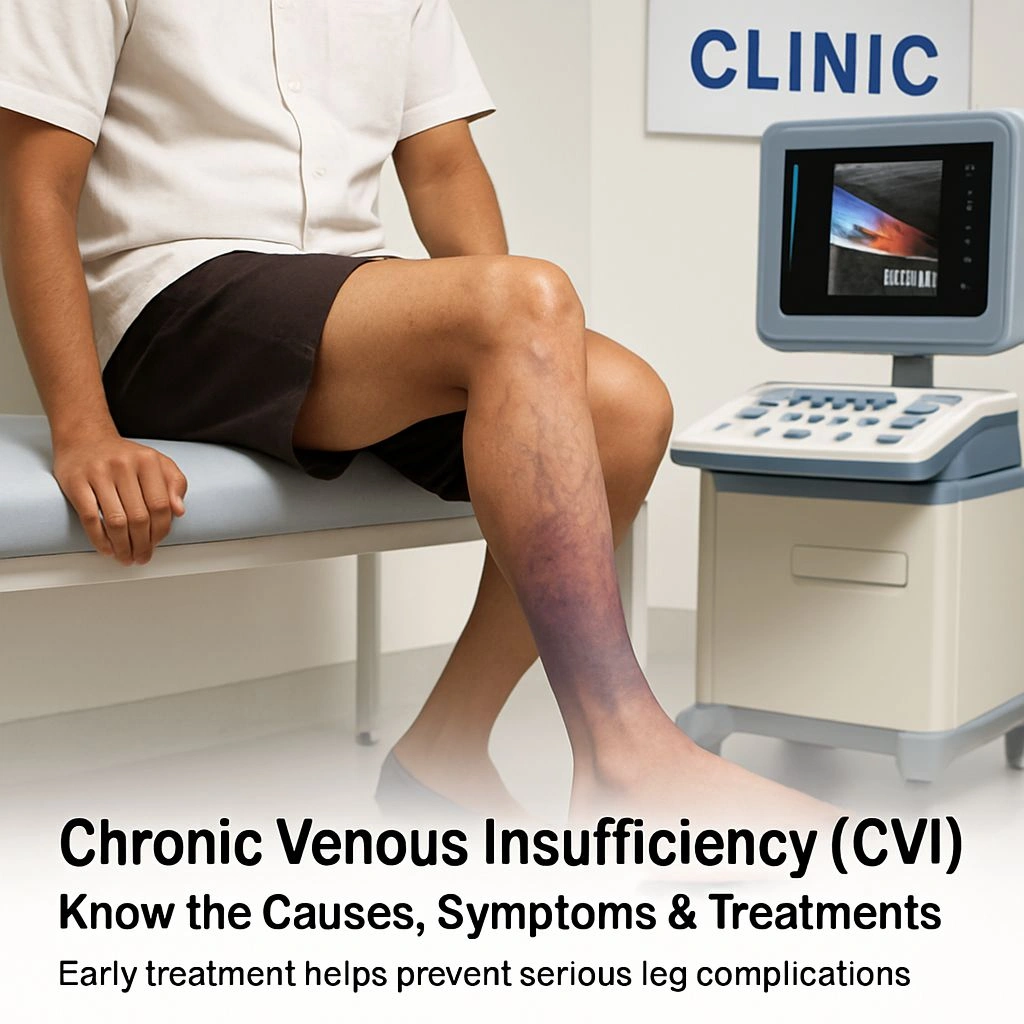
Chronic Venous Insufficiency has become a significant circulatory concern in 2025, more so among working adults and the elderly.
In case of persistent leg sensations of heaviness, swelling, or skin changes, maybe you might be dealing with Chronic Venous Insufficiency.
Being a concern of millions in India and beyond, the increasing sedentary lifestyles and late diagnoses have brought more attention to it in 2025. This happens when the veins of your legs cannot properly send blood to the heart because of valve damage.
Over time, this causes the venous reflux disease, discolorations of the leg, and eventually venous leg ulcers. If proper time awareness is created, then one could ideally treat it and stop progression.
🩺 Causes of Chronic Venous Insufficiency?
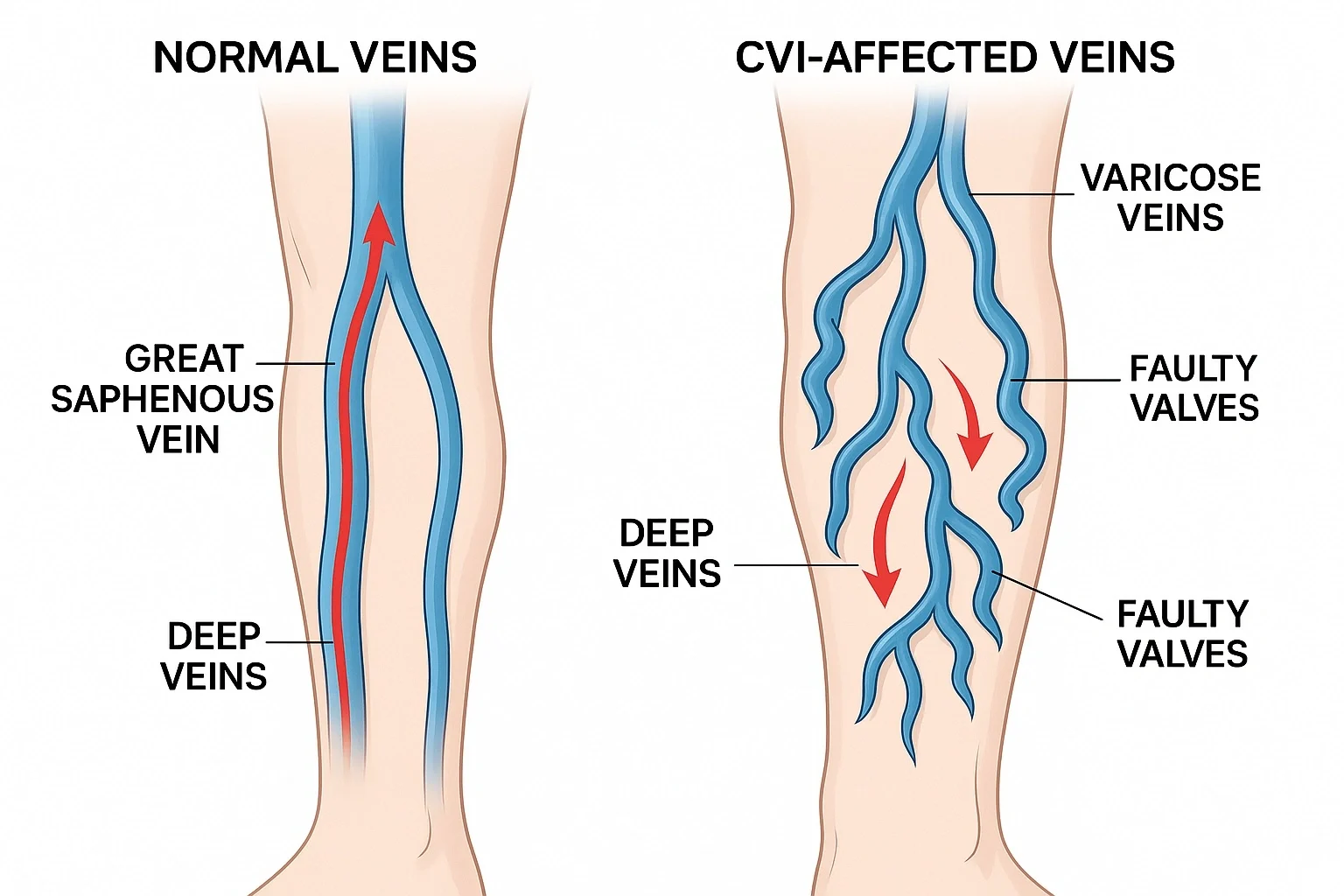
Failure of the vein valves in the legs is the main cause of chronic venous insufficiency. These faucets generally help backward inflow of blood.
In the decaying of these faucets, blood pools in the legs, thereby causing coronary pressure, dilation of modes, and aggravations.
Major causes include:
- Valve damage from deep vein thrombosis (DVT)
- Obesity and prolonged sitting/standing
- Pregnancy
- Genetic predisposition
- Trauma or surgeries in the leg region
🔬 "CVI Stage CEAP" Explained:
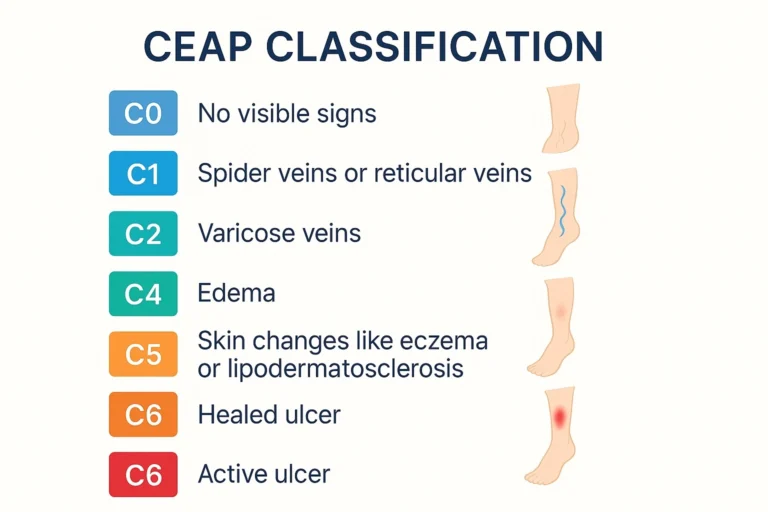
CEAP Stages:
Doctors use the CEAP (Clinical, Etiological, Anatomical, and Pathophysiological) classification system to grade the severity of CVI:
- C0 – No signs visible
- C1 – Spider veins or reticular veins
- C2 – Varicose veins
- C3 – Edema
- C4 – Skin changes like eczema or lipodermatosclerosis
- C5 – Healed ulcer
- C6 – Active ulcer
Knowing your CVI stage in CEAP helps in choosing the right treatment. For instance, those with C3–C6 might have to go for advanced treatments such as compression therapy for CVI or even surgery.
🔍 Common Symptoms and Early Warning Signs:
Signs and symptoms of Chronic Venous Insufficiency frequently progress unnoticed. You might face the following initially:
- Aching or tired legs after standing
- Swelling around the ankles
- Skin discoloration or hardening
- Inciting itching or burning
- Blue veins that appear visibly or corona phlebectatica
Advanced Symptoms:
Poor blood circulation with progression in legs may cause lipodermatosclerosis — the skin becomes tight, shiny, and painful, mostly near the lower calf.
Don’t ever ignore warning signs. One can halt worsening rigors and avoid complications if caught in time.
⚠️ Complications of Chronic Venous Insufficiency: What Happens If CVI Is Left Untreated

Venous leg ulcers are one of the most painful conditions. Uneven blood flow and skin deterioration brought on by CVI result in open wounds. These ulcers:
- Take weeks or months for healing
- Are susceptible to infections
- Reduce mobility and quality of life
These complications drastically reduce quality of life, increase healthcare costs, and cause chronic pain.
Healing becomes harder at later CVI stages CEAP, so early prevention and skin care are crucial.
✅ 7 Proven Treatment Strategies for CVI (Stage‑Based)
Treatment depends on the CVI stages CEAP and health conditions. Following are 7 evidence-based strategies:
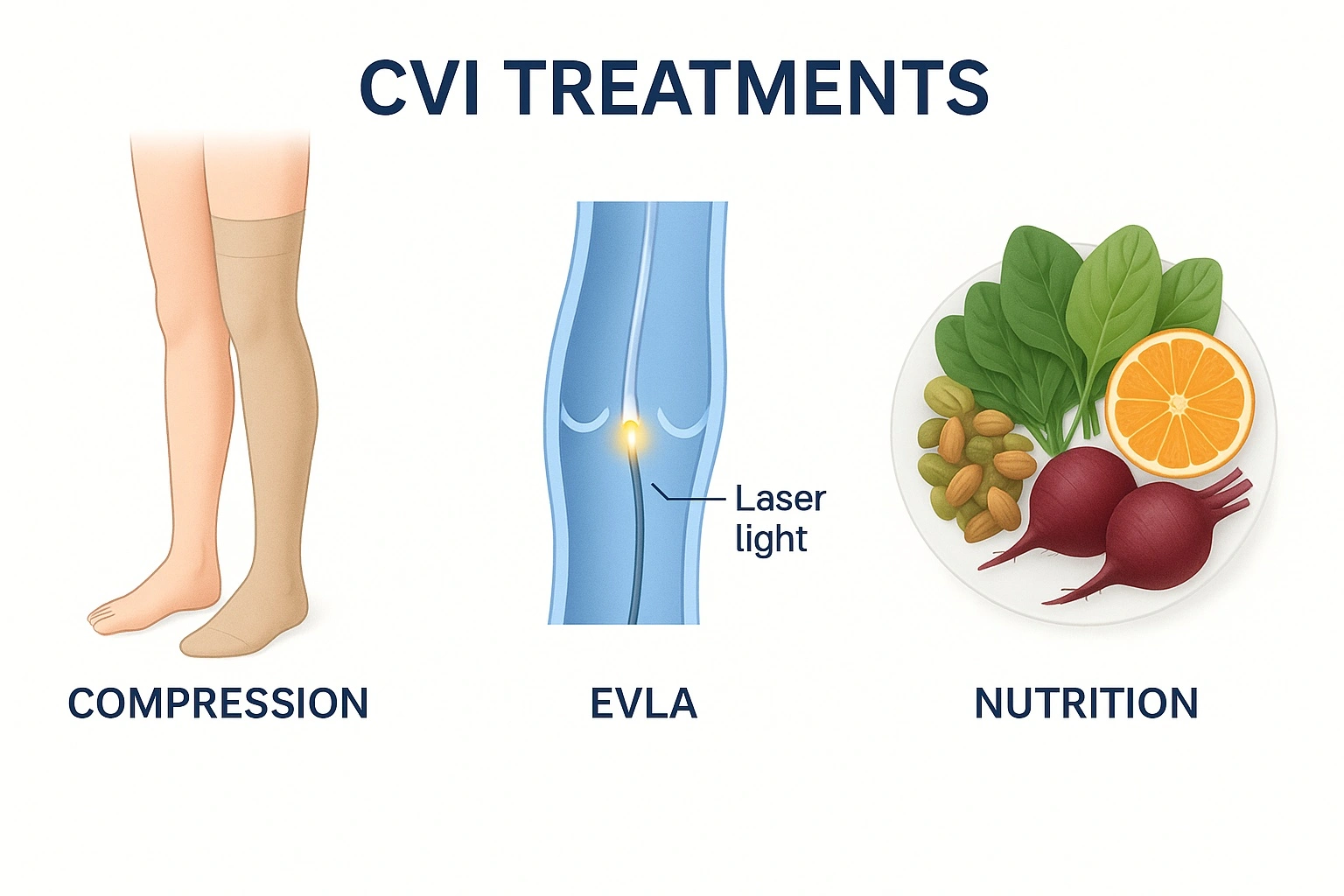
1. Compression Therapy for CVI:
Best for blood flow: stockings with medical-grade compression.
Generally available in big cities of India and through web stores.
2. Lifestyle Changes:
Walk every day, raise your legs for some time, and try to avoid long stands/sits.
3. Minimally Invasive Procedures:
EVLA or RFA is done to close the defective veins.
4. Sclerotherapy:
In order to reduce varicose veins, a chemical is injected into them (optimal for CEAP C2-C3).
5. Surgical Methods:
For complex cases (usually C5-C6), if all else fails.
6. Nutritional Therapy:
Eat a diet with flavonoids (citrus fruits, dark chocolate, green tea) to treat inflammatory conditions.
7. Herbal Therapy:
Horse chestnut extract, Butcher’s broom, and Gotu kola might help if taken under professional supervision.
In India, there are several CVI clinics across metro cities, such as Delhi, Mumbai, Jaipur, and Sikar, where one can obtain diagnoses, Doppler ultrasounds, and stocking fittings at affordable rates.
Recovery is beyond just medical treatment. It is nutritional and emotional as well. One should drink 8+ glasses of water daily to thin the blood and to keep it from clotting.
An antioxidative diet supports vascular strength. Include Impatient:
- Berries
- Onions
- Apples
- Broccoli
- Green tea
And that is not to discount the emotional element of Chronic Venous Insufficiency — body image concerns, anxiety, or frustration are almost commonplace. Resilience can be built through support groups, counseling, or light meditation.
📍Where To Find CVI Treatment In India
Getting your treatment across India would be the easiest cut. Go for:
- Doppler vascular tests at multispecialty hospitals
- CVI conventions in India like AIIMS, Fortis, and Gurukripa Hospitals (Sikar), etc.
- Certified vendors for compression stockings
Treatment cost varies between introductory contraction remedy and ray procedures, depending on the stage.
Recurrence is very much possible even after a successful treatment. A few tips for healthy legs are:
- Walking or yoga
- Skin moisturization (especially near ankles)
- Wear stocking-style compression while travelling
- Try not to cross your legs or remain in one position for too long.
- Regular follow-up every 6–12 months by a vascular doctor
📝 Conclusion: Take Action Before It Gets Worse
Chronic venous insufficiency is more than just feeling that the legs have been kept too long. Left unchecked, it goes into ulcers, infections, and permanent skin damage. But once Americans become aware, get an early diagnosis, and undergo treatment, they have a chance to regain control of their leg health.
👉 If any symptom shows up, the sooner you get a vascular specialist in the picture, the better. Don’t let it deteriorate. Prevention and early intervention are your best friends.
Frequently Asked Questions (FAQs) on Chronic Venous Insufficiency:
A. It is literally a system of classification from C0 to C6 which determines the severity of Chronic Venous Insufficiency in terms of clinical signs, its causes, and anatomically.
A. When ulcers are not healing or there are severe refluxes after failed conservative treatment (CEAP C5–C6).
A. Clean ulcers daily with saline, apply prescribed ointments, use compression, and refer to a wound care center.
symptoms are at their worst.
A. They help control symptoms and slow progression, especially in early stages; however, they will not repair valve damage.
A. Yes, family history increases risk. The major contributing factors are genetics, lifestyle, and weight.





